The Sequence of Events Leading to Infections in Healthcare Settings
Healthcare-associated infections (HAIs), also known as nosocomial infections, pose a significant risk to patients receiving medical care. These infections can occur in various healthcare settings, including hospitals, surgical centers, and long-term care facilities. Understanding the sequence of events that leads to these infections is crucial for prevention and control measures. This article will explore the mechanisms behind HAIs, the factors that contribute to their occurrence, and strategies for minimizing their impact.
Understanding Healthcare-Associated Infections (HAIs)
Definition of HAIs
Healthcare-associated infections are infections that patients acquire while receiving treatment for medical or surgical conditions in a healthcare facility. These infections can occur during hospitalization or after discharge and can be caused by various pathogens, including bacteria, viruses, and fungi.
Common Types of HAIs
HAIs can manifest in several forms, including:
- Surgical Site Infections (SSIs): Infections that occur at the site of a surgical procedure.
- Catheter-Associated Urinary Tract Infections (CAUTIs): Infections that occur in the urinary tract due to the use of catheters.
- Central Line-Associated Bloodstream Infections (CLABSIs): Infections that occur when bacteria enter the bloodstream through a central line.
- Ventilator-Associated Pneumonia (VAP): Pneumonia that develops in patients who are on mechanical ventilation.
- Gastrointestinal Infections: Infections caused by pathogens such as Clostridium difficile, often associated with antibiotic use.
Statistics on HAIs
According to the Centers for Disease Control and Prevention (CDC), approximately 1 in 31 hospital patients has at least one healthcare-associated infection on any given day. HAIs contribute to significant morbidity, mortality, and healthcare costs, with estimates suggesting that they cause 99,000 deaths annually in the United States.
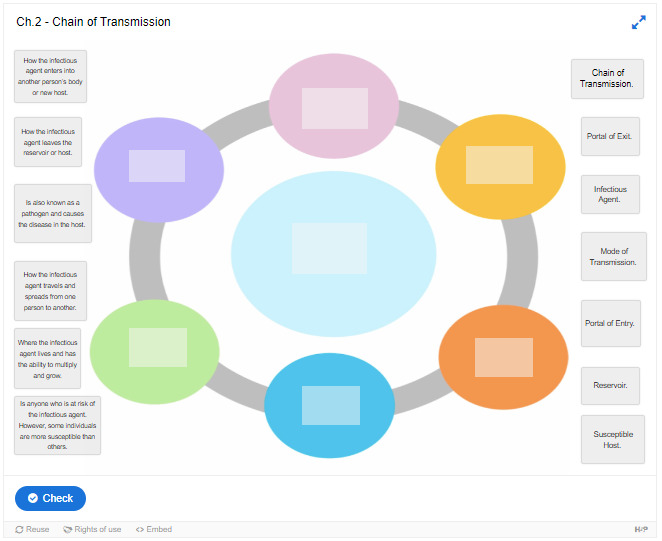
The Sequence of Events Leading to HAIs
The occurrence of HAIs can be understood through a sequence of events that involves several key components. The following sections outline these components in detail.
1. Infectious Agent
The first link in the chain of infection is the infectious agent. This includes any pathogen capable of causing disease, such as bacteria, viruses, fungi, or parasites. Common pathogens responsible for HAIs include:
- Staphylococcus aureus (including MRSA)
- Escherichia coli (E. coli)
- Clostridium difficile (C. diff)
- Pseudomonas aeruginosa
- Klebsiella pneumoniae
2. Reservoir
The second link in the chain is the reservoir, which refers to the environment where the infectious agent lives and multiplies. In healthcare settings, reservoirs can include:
- Patients: Infected individuals can serve as reservoirs for pathogens.
- Healthcare Personnel: Staff members can carry pathogens on their skin or clothing.
- Medical Equipment: Contaminated instruments and devices can harbor infectious agents.
- Environmental Surfaces: Floors, walls, and furniture can serve as reservoirs for pathogens.
3. Portal of Exit
The portal of exit is the path by which the infectious agent leaves the reservoir. Common portals of exit in healthcare settings include:
- Open Wounds: Surgical incisions or pressure ulcers can provide a route for pathogens to exit.
- Respiratory Tract: Coughing or sneezing can release infectious droplets into the air.
- Urinary Tract: Catheters can create an exit point for pathogens.
4. Mode of Transmission
The mode of transmission refers to how the infectious agent is transferred from the reservoir to a susceptible host. Common modes of transmission in healthcare settings include:
- Direct Contact: Physical contact with infected individuals or contaminated surfaces.
- Indirect Contact: Transmission through contaminated objects (fomites) or surfaces.
- Airborne Transmission: Pathogens can be inhaled through respiratory droplets.
- Vector-Borne Transmission: In some cases, insects or animals can transmit infections.
5. Portal of Entry
The portal of entry is the route through which the infectious agent enters a new host. Common portals of entry include:
- Skin: Breaks in the skin can allow pathogens to enter.
- Respiratory Tract: Inhalation of infectious droplets can lead to respiratory infections.
- Gastrointestinal Tract: Ingestion of contaminated food or water can introduce pathogens.
6. Susceptible Host
The final link in the chain is the susceptible host, which refers to individuals who are at risk of infection. Factors that contribute to susceptibility include:
- Immunocompromised Individuals: Patients with weakened immune systems due to illness or medication.
- Age: Elderly individuals and very young children are more vulnerable to infections.
- Chronic Conditions: Patients with chronic illnesses, such as diabetes or heart disease, may be more susceptible.
Breaking the Chain of Infection
To prevent HAIs, it is essential to break the chain of infection at any of the links mentioned above. Here are some effective strategies:
1. Hand Hygiene
Proper hand hygiene is one of the most effective ways to prevent the spread of infections in healthcare settings. Healthcare personnel should wash their hands frequently and use alcohol-based hand sanitizers when appropriate.
2. Use of Personal Protective Equipment (PPE)
Wearing appropriate PPE, such as gloves, masks, and gowns, can help protect healthcare workers and patients from exposure to infectious agents.
3. Environmental Cleaning and Disinfection
Regular cleaning and disinfection of surfaces, medical equipment, and patient areas can help reduce the presence of pathogens in healthcare settings.
4. Sterilization of Medical Instruments
All surgical and invasive instruments should be properly sterilized before use to eliminate any potential pathogens.
5. Safe Injection Practices
Healthcare providers should follow strict protocols for safe injection practices to prevent infections associated with injections.
6. Patient Education
Educating patients about infection prevention measures, such as hand hygiene and recognizing signs of infection, can empower them to take an active role in their care.
Conclusion
Healthcare-associated infections are a significant public health concern that can lead to serious complications and increased healthcare costs. Understanding the sequence of events that leads to HAIs is crucial for healthcare professionals and patients alike. By recognizing the links in the chain of infection and implementing effective prevention strategies, we can work together to reduce the incidence of these infections and improve patient outcomes.
Frequently Asked Questions (FAQ)
Q1: What are healthcare-associated infections (HAIs)?
HAIs are infections that patients acquire while receiving treatment for medical or surgical conditions in a healthcare facility.
Q2: What are common types of HAIs?
Common types of HAIs include surgical site infections (SSIs), catheter-associated urinary tract infections (CAUTIs), central line-associated bloodstream infections (CLABSIs), and ventilator-associated pneumonia (VAP).
Q3: How can HAIs be prevented?
HAIs can be prevented through proper hand hygiene, the use of personal protective equipment (PPE), environmental cleaning and disinfection, sterilization of medical instruments, safe injection practices, and patient education.
Q4: Who is at risk for HAIs?
Individuals at higher risk for HAIs include those with compromised immune systems, the elderly, infants, and patients with chronic conditions.
Q5: What role do healthcare providers play in preventing HAIs?
Healthcare providers are responsible for adhering to infection control protocols, educating patients, and implementing best practices to minimize the risk of HAIs.
Summary Table
| Aspect | Description |
|---|---|
| Definition of HAIs | Infections acquired during healthcare treatment |
| Common Types of HAIs | SSIs, CAUTIs, CLABSIs, VAP |
| Key Prevention Strategies | Hand hygiene, PPE, cleaning, sterilization |
| High-Risk Populations | Immunocompromised, elderly, chronic conditions |
| Role of Healthcare Providers | Adhere to protocols, educate patients |
For more information on healthcare-associated infections, you can refer to the Centers for Disease Control and Prevention (CDC) website.